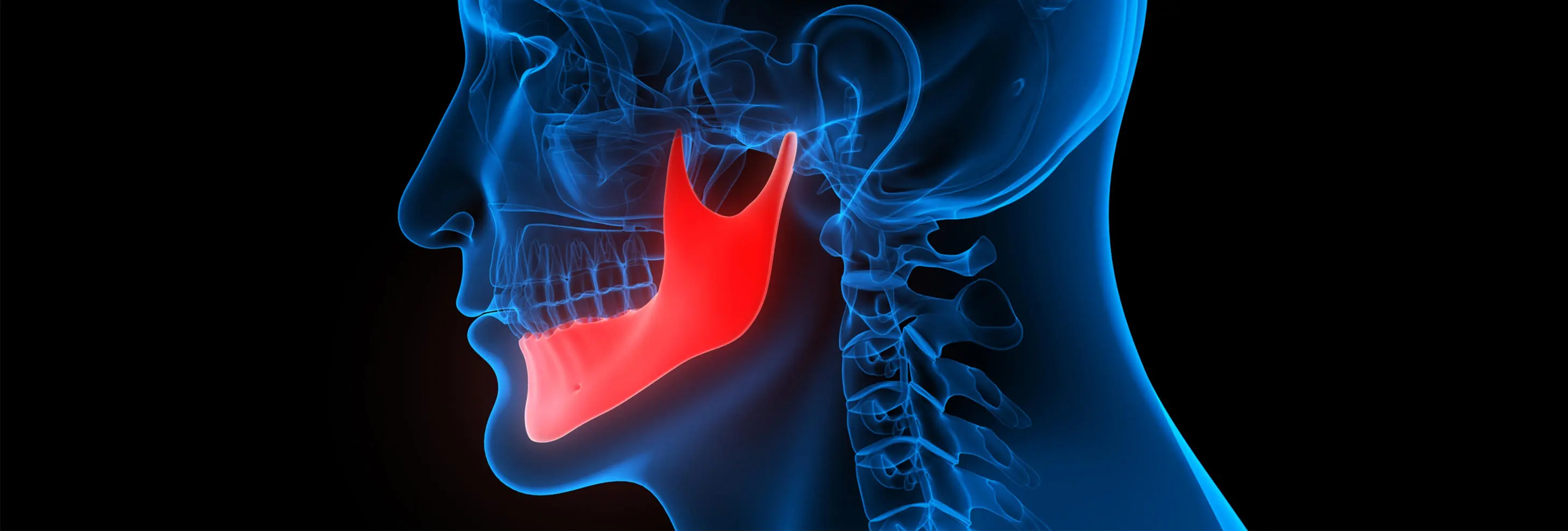
Two institutions will investigate the use of antibiotics post lower jaw surgery
The University of Central Lancashire (UCLan) and East Lancashire Hospitals NHS Trust (ELHT) has been awarded nearly £2 million to undertake a collaborative antibiotics research project.
The two institutions will use the £1.87m National Institute for Health Research grant to investigate if patients with lower jaw fractures should be given antibiotics following surgery.
Led by ELHT’s Professor Panayiotis Kyzas, the study will recruit 2,907 adult patients, from NHS Oral & Maxillofacial Surgery units across the country, who have broken their lower jaws and require surgery to repair the damage.
Professor Kyzas said: “The aim of this study is to find out if patients having an operation to fix a lower jaw fracture are less likely to get an infection if given antibiotics after their surgery.
"Cutting into the mouth to fix these fractures puts the patient at risk of infection, which affects 1 in 10 cases"
— East Lancashire Health Trust's Professor Panayiotis Kyzas
“There are more than 6,000 lower jaw fractures per year in the UK and they are the most common facial fractures needing surgery. Cutting into the mouth to fix these fractures puts the patient at risk of infection, which affects 1 in 10 cases. Infection requires treatment with antibiotics, may need further surgery and can cause long-term jaw pain, jaw malalignment and dysfunction.
“Surgeons give antibiotics at the start of the operation to reduce the chance of an infection. However, research suggests that antibiotics given after surgery may not necessarily reduce the risk of infection in patients with a lower jaw fracture. There is wide variation in current clinical practice and that is why we want to investigate this important area.”
Currently, practice is much more standardised for other facial fractures.
UCLan’s Clinical Trials Unit will undertake the vast majority of the work to compare three different antibiotic approaches following surgery.
"Reducing and optimising antibiotic use is very important for individual patient health and the wider NHS"
— Professor Dame Caroline Watkins, the Director of UCLan’s Lancashire Clinical Trials Unit
Participants will be randomly assigned to one of three groups. One will receive no further antibiotics after surgery, the second will receive two further doses of intravenous antibiotics after surgery while the third group will receive two further doses of intravenous antibiotics and five days of oral antibiotics.
All three patient groups will follow the normal care pathway and receive the same usual treatment and each patient will be followed up at 14, 30 and 180 days after surgery.
Professor Dame Caroline Watkins, the Director of UCLan’s Lancashire Clinical Trials Unit, said: “Reducing and optimising antibiotic use is very important for individual patient health and the wider NHS. Good antibiotic stewardship is critical to reducing antibiotic-related complications and future antibiotic resistance.
“Therefore, this study will try to answer four questions. Does changing the amount of antibiotics that a patient receives after surgery for a mandible fracture change their risk of getting an infection? Is there any difference in cost of the different antibiotic approaches? How do patients and health professionals feel about a change to current clinical practice? How could we best communicate the findings of the study in order to make changes to NHS clinical practice in the future?”